How Emergency Psychiatric Intervention Works
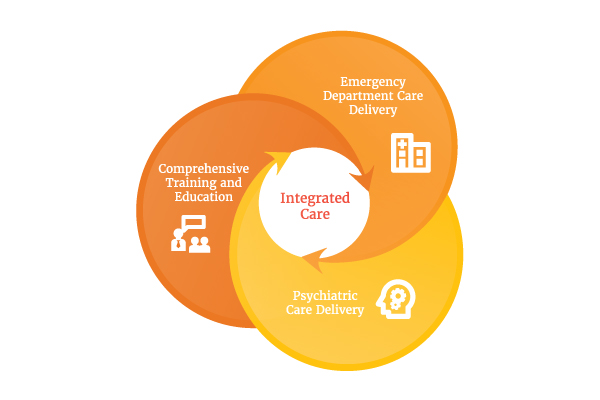
At its core, the EPI approach includes expertise and proven results in three areas:
- Elimination of over-processing
- Risk stratification and split flow processing
- Early and appropriate medication management
These three principles are already embedded in the standard processes that serve patients with medical complaints in the ED. However, they have not been successfully applied to the behavioral health population.
Through the elimination of unnecessary roadblocks to expedite treatment, patients receive earlier assessments and differentiated care based on diagnosed need. Also, EPI creates core efficiencies to assess, evaluate, and treat behavioral health patients, reducing redundancies and freeing up time to care for more patients. All of this is achieved through a comprehensive education program and toolkit on behavioral healthcare best practices that minimize patient holding and improve care quality and patient experience.
Transforming the ED for All Stakeholders
The impact of effectively and compassionately serving all ED patients, including those with behavioral health conditions, is profound.
- Hospitals and health systems improve clinical quality, profitability, and patient scores while elevating their brand.
- EDs achieve higher throughput and better care for all, with fewer behavioral patient admissions and more stable, engaged staff.
- Providers gain new confidence in their ability to heal, rekindling the joy of practicing medicine.
- All patients know on a very human level that they're properly cared for with dignity and respect.
Implementing EPI requires formalized training for emergency providers as well as access to dedicated behavioral health services. To learn more, contact [email protected].